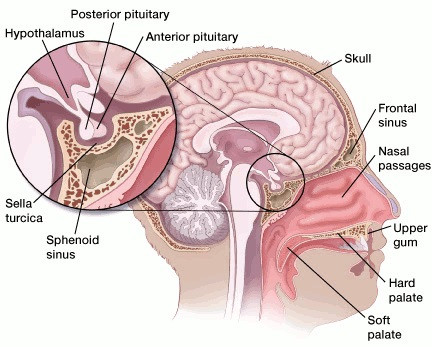
The pituitary is the master gland situated immediately beneath the brain. It controls most hormone-producing glands, such as the thyroid and adrenals.
Pituitary tumours (also known as pituitary adenomas, pituitary neuroendocrine tumours or ‘pitNETs’) are relatively common, affecting 1 in 1000 people and accounting for 15% of all tumours of the central nervous system.
Pituitary tumours cause headaches, loss of vision and serious systemic health problems due to hormone excess or deficiency. The most common type of pituitary adenoma is prolactinoma, comprising >60% of all cases, and being particularly prevalent in reproductive-age people.
South Australia has an expert multidisciplinary team of clinician-researchers working on novel solutions to improve the diagnosis and management of pituitary tumours. Projects to date include surgical training techniques to improve pituitary surgery expertise, identification of new pituitary tumour predisposition genes and studies of the toxicities associated with dopamine agonists (e.g., cabergoline) in the treatment of prolactinomas. These projects have been featured in major international guidelines.
With your support, we can continue our innovative research to provide more diagnostic and treatment options for people with pituitary tumours in South Australia and beyond.
2025 Research Funded:
Funding: $30,000
Part 1: Characterisation of the differences in membrane receptor proteins between normal pituitary gland and pituitary adenomas: Possible targets for fluorescence guided surgery.
Part 2: Histological examination of tumour fibrosis in cabergoline-treated prolactinomas.
Non functioning pituitary adenomas are a common clinical problem that can threaten the nerves involved with vision. These tumours arise in the pituitary gland which controls multiple hormonal functions. Surgery to remove these tumours can be performed, but carries the risk of damage damage to the normal pituitary gland, which can result in hormonal dysfunction. It can be difficult to tell between the adenoma and normal pituitary gland intraoperatively, and our study represents a first step in developing techniques to make this easier.
One approach is to investigate how the membrane receptors found on pituitary adenomas differ from normal pituitary gland. Our previous work has shown that it is likely there are some differences between them, but if we could demonstrate which receptors are different that could represent a possible target for a fluorescent molecule, which could be used to identify residual tumour at the time of surgery.
An additional approach we are taking is to investigate the intrinsic fluorescent behaviour of both adenoma tissue and normal gland. We know from prior research that the pituitary gland fluoresces under light of a certain wavelength. We want to test whether pituitary adenoma tissue fluoresces under light of this wavelength or not. If it does not, this again represents a further way of differentiating between tumour and normal gland at the time of surgery.
Finally, we will be assessing whether preoperative treatment of a prolactinoma (a type of pituitary adenoma) with a drug called cabergoline induces fibrosis (scar tissue formation) in the prolactinoma. This scar tissue makes the prolactinoma firmer and more difficult to safely remove at the time of surgery. Our findings will have implications for how these tumours are managed moving forwards: If we find that treatment with this medication does not induce fibrosis, it may support the fact that a trial of medical treatment in the first instance for these cases is a reasonable approach.

Dr Chris Ovenden, MBBS, Neurosurgery Registrar
Abbie Simpson Clinical Fellow
PhD Candidate - University of Adelaide, Department of Surgical Sciences.
Funding: $50,000
F-FDOPA PET/CT for the identification of prolactinomas and prediction of dopamine agonist treatment response: development of a novel molecular imaging scan for pituitary tumours. Tumours of the pituitary gland (located beneath the brain) are common, affecting 1/1000 people. Prolactinomas (defined by hypersecretion of prolactin hormone) are the most frequent pituitary tumour subtype. Currently, no functional imaging tests are available for the diagnosis of prolactinomas. In this world-first study, we will assess the ability of a radiotracer, F-FDOPA, to provide functional information about these tumours and aid in their diagnosis. Here, we will demonstrate its ability to diagnose prolactinomas and inform management decisions e.g., surgical planning and responsiveness to medications.

Dr James McNeil, MBBS FRACP FAANMS
Nuclear Medicine, Royal Adelaide Hopsital

A/Prof Sunita De Sousa, MBBS MSc PhD FRACP
Endocrinology & Clinical Genetics, Royal Adelaide Hospital
2023 Research Funded:
Funding: $64,000
Endoscopic endonasal transsphenoidal surgery (EETS) to remove pituitary adenomas is now an accepted approach since first being described in 1992. Over the last 30 years the complications associated with endoscopic transsphenoidal surgery has dramatically improved, namely rates of CSF leak, visual outcomes and degree of tumour resection. Post operative endocrinopathy from damage to the pituitary gland and/or stalk does not appear to have reduced overtime at a similar rate to other complications. This research project would examine the South Australian experience with EETS and determine if the same relationship exists between surgeon experience and rates of post operative endocrinopathy. Furthermore, the accuracy of neuronavigation in skull base surgery will be quantified and identification of the difference in membrane receptor expression between pituitary glad and pituitary tumour will be examined.

Dr Nick Candy Neurosurgical Accredited Registrar and PhD in Surgery Student
ABBIE SIMPSON CLINICAL FELLOW
Feb-24 Candy NG, Jukes AK, Van Der Veken J, Torpy DJ, Vrodos N, Santoreneos S, Wormald PJ, Psaltis AJ. The Learning Curve for Endoscopic Endonasal Transsphenoidal Pituitary Surgery: Evaluating Endocrine Outcomes. Journal of Clinical Neuroscience. 2024 Feb 1;120:14-22.
Apr-24 Candy NG, Jukes AK, Ooi EH, Valentine R, Vrodos N, Santoreneos S, Floreani S, Wormald PJ, Psaltis AJ. The Evolution of Pituitary Surgery in an Australian Health Care Framework. Journal of Neurological Surgery Part B: Skull Base. 2024 Apr 15.
Apr-24 De Sousa SMC, McCormack A, Orsmond A, Shen A, Yates CJ, Clifton-Bligh R, Santoreneos S, King J, Feng J, Toubia J, Torpy DJ, Scott HS. Increased prevalence of germline pathogenic CHEK2 variants in individuals with pituitary adenomas. Journal of Clinical Endocrinology & Metabolism. 2024 Apr 23:dgae268.
Apr-24 Mathew A, Gorayski P, Candy N, Saran F, Le H. Proton beam therapy for clival chordoma: Optimising rare cancer treatments in Australia. Journal of Medical Radiation Sciences. 2024 Apr;71:47-58.
May-24 Candy NG, Jukes AK, Patel S, King T, Bouras G, Vrodos N, Wormald PJ, Psaltis AJ. Neuronavigation in endoscopic skull base surgery and the accuracy of different MRI sequences. Journal of Clinical Neuroscience. 2024 May 1;123:203-8.
May-24 De Sousa SMC, Jukes AK, Candy NG, Chapman IM, Torpy DJ, Shivalingam B, Wormald PJ, Santoreneos S. Tumour fibrosis in dopamine agonist-exposed prolactinomas is a diminishing concern. Nature Reviews Endocrinology. 2024 May;20(5):314-.
Oct-24 Candy NG, Santoreneos S, Wormald PJ. Pseudocapsular dissection in a large plurihormonal Pit-1 positive PitNET. October 2024. Journal of Clinical Neuroscience.
Dec-24 Candy NG, Ramezanpour M, Bouras G, Chegeni N, Chataway T, Ormsby RJ, Jukes AK, Vreugde S, Wormald PJ, Psaltis AJ. Differential proteomic expression in non-functional pituitary neuroendocrine tumours and pituitary glands. Rhinology.2024 Dec 1;62(6):750-758.
Dec-24 Mignone E, Jukes A, Valentine R, Allison R, De Sousa SMC. Aripiprazole use as a cause of dopamine agonist failure in the treatment of prolactinomas. Endocrine Oncology. 2024 Dec 1;1(aop).
Jul-24 Neurosurgical Research Foundation Research Grant ($50,000)
Aug-24 Australian Nuclear Science and Technology Organisation/ANZ Society of Nuclear Medicine Research Grant ($20,000)
Nov-24 Endocrine Society of Australia Seed Grant ($10,000)
Nov-24 Endocrine Society of Australia-Clinical Endocrinology Journal Early Career Award
Nov-24 Endocrine Society of Australia Paul Lee Best Abstract Award
Nov-24 Endocrine Society of Australia Young Investigator Award