Dementia and Parkinson’s disease are the two most common neurodegenerative diseases. And while dementia is the second leading cause of death in Australia with one new case every six minutes, and Parkinson’s disease affects over 200,000 Australians, there is no treatment – only options to relieve symptoms.
Before they can find a cure, researchers need to better understand how neurodegenerative diseases develop.
Without a medical breakthrough, the number of Australians living with dementia is set to soar from 413,106 to 900,000 by 2050. Parkinson’s disease cases are also expected to double by 2030 as our population ages, currently costing the Australian economy more than $1.1 billion each year.
With your support, we can fund urgent research into Parkinson’s disease and dementia treatments.
2025 Research Funded:
Funding: $47,111
Parkinson’s disease (PD) is one of the most common neurodegenerative disorders, driving significant disability in more than 100,000 Australians. Although several therapies for PD exist, these have many side-effects and will eventually fail in most patients. Consequently, next generation therapies that are minimally invasive, low risk and reliable are required. This project will address this problem by developing a novel, non-invasive brain stimulation technique that targets pathological patterns of brain activity that have been associated with symptom development. This will pave the way for clinical investigation of new therapeutic interventions.
Dr George Opie, PhD, Senior Research Fellow
The University of Adelaide, Physiology, School of Biomedicine.
Funding: $50,000
The 1 year, 0.8 FTE post-doctoral Research Assistant (RA) position will lead biomarker/PET analysis as part of the ongoing FIND-TBI study and investigate the role of neuroinflammatory and dopaminergic alterations in driving persistent function impairment following traumatic brain injury. TBI significantly increases risk of later developing a neurodgenerative disorder, including Parkinson’s disease (PD).
During this post-doctoral fellowship, the candidate will examine blood- and saliva-based markers of neurodegeneration and neuroinflammation, as well as alterations in dopamine and neuroinflammatory signaling on PET imaging, in individuals following different severities and at different time points post-TBI. Such markers could act as critical indicators of who is most at risk of developing PD, long before clinical onset.
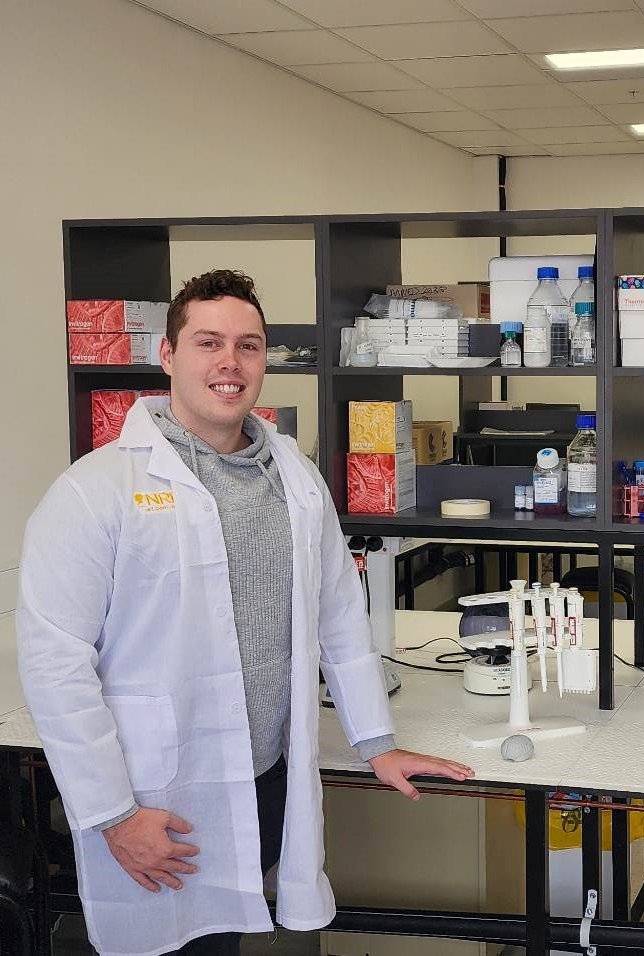
Angus McNamara
Level A Post-doctoral fellow, Translational Neuropathology Laboratory, School of Biomedicine, The University of Adelaide
Funding: $50,000
A research assistant is required for an in-vivo investigation of the relationship between head accelerations during contact sports and changes in microstructural neuroanatomy and cognitive function. The targeted RA has uniquely relevant expertise and experience and will manage all participant scheduling, data collection, and brain MRI scan data post-processing.
Repeated head trauma has long been associated with increased risk of neurodegenerative disease, especially among contact sport athletes. Over the last decade, sporting authorities have endeavoured to reduce athlete exposure to repeated head trauma by implementing head injury assessment and concussion protocols; however, current screening tools are largely subjective and fail to account for repetitive sub-concussive events.
In the current longitudinal study, 6 amateur rugby players without history of significant TBI will be recruited. Over the competitive sporting season (6-8 months) the head acceleration events will be measured via a custom-fit HitIQ instrumented mouthguard. Repeated brain MRI scans will be performed
Hugh McCloskey
Centre for Orthopaedic and Trauma Research & Adelaide
Spinal Research Group, Adelaide Medical School, The
University of Adelaide
Funding: $50,000
Sleep and circadian rhythm disturbances are central features of many neurological disorders including Parkinson’s disease, Alzheimer’s disease and depression. Furthermore, it is becoming increasingly evident that there is a bidirectional relationship between sleep and neurological disorders: thus, sleep disturbances can initiate, worsen and/or facilitate progression of neurological disorders, while many neurological disorders result in poor sleep quality. The mechanisms of these bidirectional relationships are not established.
The system monitors and analyses data related to sleep/wake cycles. This system is totally non- invasive and does not require surgery. Automated sleep-wake scoring reduces costs.
We will be able to measure sleep-wake cycles, sleep disturbances, breathing-related parameters and the circadian changes in models of neurological disorders non-invasively for the first time. To the best of our knowledge, this will be the first system in Australia that will allow these measurements completely non-invasively using this novel technology.
This equipment will support multiple projects between three South Australian universities using preclinical models of diseases that aim to investigate
1) the bidirectional relationships between sleep and neurological disorders;
2) the effects of novel drugs on sleep and circadian rhythms in neurological disorders;
3) the interactions between sleep, diet and gut microbiome in neurological disorders.
![]()
A/Prof Larisa Bobrovskaya, Clinical and Health Sciences
University of South Australia
2024 Research Funded:
Funding: $49,848
In our laboratory we investigate the role of specific neurons (called orexin neurons) in PD. The orexin neurons can influence multiple functions throughout the body including motor control, sleep-wakefulness, memory, cognition, mood and gastrointestinal function. Orexin neurons are damaged in PD, however, our knowledge about the causal contribution of orexin neurons in PD is very limited. Thus, further research is urgently needed.
A/Prof Larisa Bobrovskaya, Clinical and Health Sciences
University of South Australia
Funding: $34,060
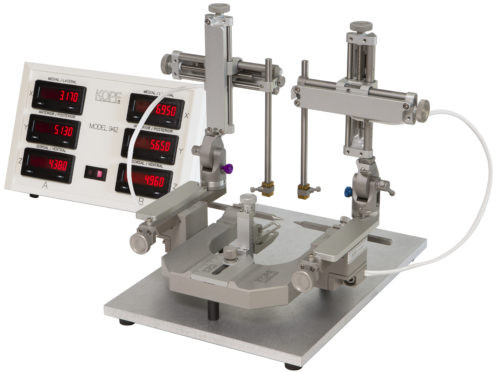
The dual-arm stereotax with digital readout allows for the generation of experimental models of neurological disease with a high degree of precision not previously possible. This equipment has broad application across multiple disease models, ranging from Parkinson's disease to stroke to traumatic brain injury, and will allow us to carry out the foundational experiments that further our understanding of disease mechanisms and bring us one step closer to translating treatment strategies from the bench to the bedside
A/Prof Lyndsey Collins-Praino PhD Interim Head of Discipline, Anatomy and Pathology Head, Cognition, Ageing and Neurodegenerative Disease Laboratory (CANDL)
The University of Adelaide - Medical Sciences
2022 Research Funded:
Funding: $13,021
Research Area: Parkinson’s
Project: Although the cause of Parkinson’s disease (PD), which currently affects 10 million people worldwide, remains to be elucidated, several risk factors have been implicated.
One of the most significant of these is a prior history of traumatic brain injury (TBI), with epidemiological studies reporting that a mild TBI increases risk of PD by 56%, whilst moderate/severe TBI increases PD risk by 83%. To date, the brain mechanisms that may explain this link are unclear. This project will investigate whether TBI increases PD risk by accelerating the pathological spread of misfolded alpha-synuclein, the pathological hallmark of PD, throughout the brain.

A/Prof Lyndsey Collins-Praino PhD Interim Head of Discipline, Anatomy and Pathology Head, Cognition, Ageing and Neurodegenerative Disease Laboratory (CANDL)
The University of Adelaide - Medical Sciences
2021 Research Funded:
Assoc Prof Lyndsey Collins-Praino
Senior Lecturer, Discipline of Anatomy and Pathology, University of Adelaide
University: Adelaide University
Funding: James & Diana Ramsay Foundation $73,229 x 3 years total $ 219,687
Project: This project will develop a comprehensive behavioural testing battery to characterise differences in the integrity of specific basal ganglia circuits involved in decision making in different subtypes of PD. Additionally, we will identify genes relevant to basal ganglia circuit function that may predict risk and progression of cognitive decline in PD.
A major contributor to the spread of Parkinson’s disease throughout the brain is the transmission of an abnormally folded protein, called alpha synuclein, from brain cell to brain cell. The aim of this project is to pioneer a novel technology to target this alpha synuclein within the extracellular space and clear it from the brain. This may help to stop the brain transmission of alpha synuclein, halting the spread of the disease, and leading to a disease-modifying treatment strategy for PD.
Assoc Prof Lyndsey Collins-Praino
Senior Lecturer, Discipline of Anatomy and Pathology, University of Adelaide
Stroke is a leading cause of death, disability and dementia worldwide. However, loss of brain tissue distal to the primary stroke site, can occur months to years following stroke, increasing patient disability. This process is called secondary neurodegeneration and the underlying mechanisms of this delayed neuronal loss remain poorly understood. Pericytes are known to be involved in the early injury pathways following stroke; however, they may also contribute to delayed neurodegeneration given their roles in maintaining blood-brain barrier structure, transport, controlling blood flow, driving new cell growth and formation of new blood vessels. Despite this, no studies have investigated the contribution of pericyte changes to secondary neurodegeneration post-stroke. Accordingly, this study seeks to further understand what drives secondary neurodegeneration and whether pericytes are key contributors to post-stroke neurodegeneration. Specifically, we will examine the course of pericyte changes following stroke and determine alterations in key neurodegenerative and neuroinflammatory markers
Assoc Prof Lyndsey Collins-Praino
Senior Lecturer, Discipline of Anatomy and Pathology, University of Adelaide
Parkinson’s disease (PD) is the second most common neurodegenerative disease after Alzheimer’s disease, affecting 10 million people worldwide and 1 in every 350 Australians. While the exact causes of PD are currently unknown, one risk factor is traumatic brain injury. Despite growing awareness of the link between TBI and PD, however, brain mechanisms that account for this relationship are unknown. One potential mechanism may be neuroinflammation. A potent inducer of neuroinflammation is activation of Toll-like receptor 4 (TLR4), a pattern recognition receptor broadly expressed in the central nervous system. The current study will investigate whether the development of neuroinflammation and PD-like pathology following TBI is mediated by TLR4 activation. This has the potential to shed light on the mechanism by which a major risk factor for PD may lead to disease, and may help to identify novel therapeutic targets.
Assoc Prof Lyndsey Collins-Praino, previously investigated how brain inflammation changes over time, and whether this is associated with brain changes characteristic of neurodegenerative diseases, such as Alzheimer’s and Parkinson’s disease. One major risk factor for these diseases is traumatic brain injury (TBI). While it is not yet clear how TBI can lead to the brain changes seen in PD, often decades after the original injury, TBI is known to be associated with the induction of significant inflammation in the brain. This may set the stage for the later emergence of neurodegenerative disease. This raises the exciting possibility that targeting inflammation after injury may help to reduce the incidence of these conditions, at least in a subset of the population.
Assoc Prof Collins-Praino is also focused on understanding the brain mechanisms that underlie cognitive impairments, such as memory problems and difficulties with planning and paying attention, in these conditions.
Dr Frances Corrigan
Senior Lecturer in Anatomy, School of Health Sciences, University of South Australia
A history of repeated concussions has been linked to three times higher risk of developing a neurodegenerative disease, to which there are currently no effective treatments. How repeated concussion promotes neurodegeneration, and what role alcohol abuse plays in that process, is poorly understood, making it difficult to intervene in the disease process. Work is ongoing to characterize the effects of chronic alcohol exposure on pathological changes following repeated concussion and determine whether this leads to long-term changes in behaviour, particularly cognition, depressive-like behaviour, and anxiety. This is particularly important given the accepted usage of alcohol within the community and the lack of understanding of what constitutes a safe level of alcohol consumption following a mild traumatic brain injury.
An especially common injury in contact sports such as football, chronic traumatic encephalopathy is a neurodegenerative disease, which appears to be exclusively related to repeated concussion.
Dr Francis Corrigan Chronic Traumatic Encephalopathy (CTE) is a neurodegenerative disease which appears to be exclusively related to repeated concussion. This research considers the mechanisms by which systemic inflammation accelerates the disease process, leading to neuronal cell death.
Dr Francis Corrigan’s research examines how concussion – particularly repeated concussion – may increase the risk of developing cognitive deficits later in life. Previous research has suggested that levels of substance P (SP) are higher in adolescents and thus they may have a greater inflammatory response to a concussive insult than an adult. We will be investigating whether blockade of this inflammatory response – by preventing the actions of SP – will prevent the development of cognitive deficits following concussion in adolescence.
Click here to donate to the Neurodegeneration Research Appeal