Medical researchers need to develop special techniques to treat children, since their brains aren’t yet fully developed and can regrow and self-heal.
With your support, we can fund Paediatric Neurosurgical Research into the treatment of brain and spinal diseases and injury. This includes toddler concussion, head injury, brain tumours and brain cancer in children.
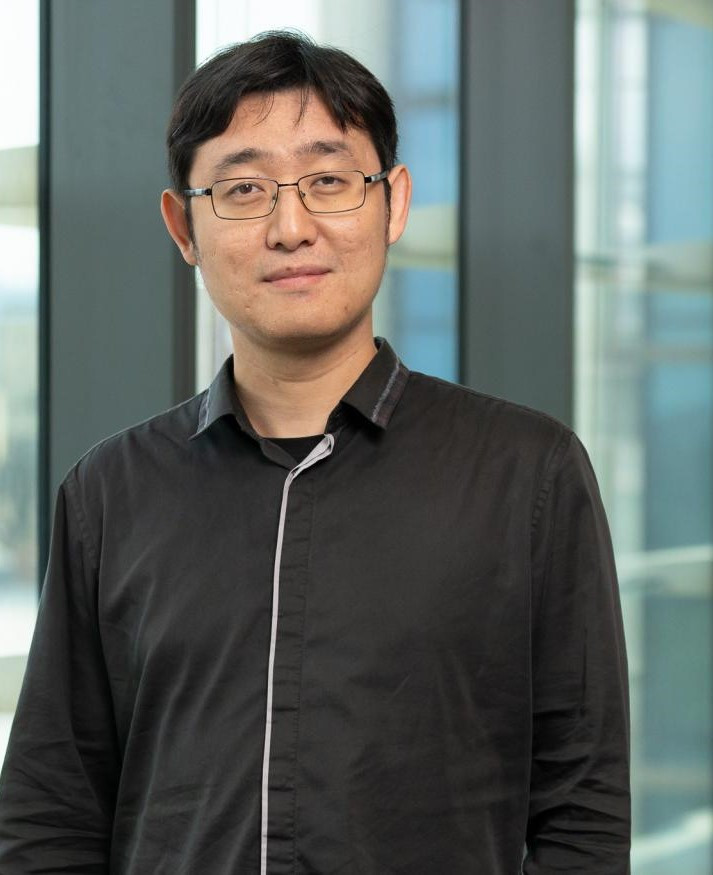
RESEARCHER: Dr Yannan Yang
FUNDING: NRF $50,000, 2024 MRFF Early to Mid-Career Researchers Grant $843,021
PROJECT: We have developed a nanorobot-based vaccines technology to improve the T cell response for solid tumours. This project will perform a preclinical study to develop and validate the nanorobot-based vaccine boosted CAR-T therapy for treating inoperable DIPG tumours.
Funding: $48,072
Brain tumours are the number 1 disease cause of death in children. The nastiest of these are the tumours that grow in the centre of the child’s brain, where they sit so close to essential, life- maintaining functions that they are impossible to operate on. We believe that new, personalised cell therapies offer a chance to treat these deadly cancers. We are manufacturing these therapies at SA Pathology for a national trial at the Sydney Children’s Hospital. Named after a patient who died of this disease, the LEVI’S CATCH trial is offering the hope of new treatment options for children with currently incurable brain tumours.

Dr Tessa Gargett, BA BSc (Hons) PhD, Research Officer, Central Adelaide Local Health Network, Translational Oncology Laboratory

Funding: $50,000
This project aims to study the radiation sensitivity of brain tumours in adults and children with Glioblastoma (GBM). We will grow and radiate tumour cells from both age groups in the lab, simulating clinical protocols. By comparing responses, we hope to understand age-related treatment effectiveness. Additionally, we will examine how the brain environment influences tumour response and create lab models to simulate the complex molecular environment of GBM. This research will enhance our understanding of tumour behaviour and treatment responses across ages.

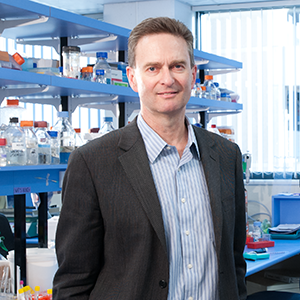
Professor Cedric Bardy PhD, ARC Future Fellow, Group Leader, Flinders University, SAHMRI
Funding: $50,000
Medulloblastoma is a common, aggressive childhood brain tumour. Currently, standard treatment consists of tumour surgical resection, chemotherapy and radiotherapy administered to the entire brain and spine. This grueling treatment regime can cause permanent and debilitating neurocognitive impairment in children, and so there is a significant need for less toxic therapies. Sphingosine kinase, a protein with known oncogenic properties, is highly expressed in a sub-type of medulloblastoma and this correlates with poorer patient survival. We hypothesise that sphingosine kinase contributes to the pathogenesis of medulloblastoma, and targeting this protein may provide an effective, safer therapy for children impacted by these tumours.

Prof Stuart Pitson BAppSc, PhD, NRF Chair of Brain Tumour Research/Head of Molecular Therapeutics Laboratory, University of South Australia, Centre for Cancer Biology
Funding: $100,000 over 3 years commencing 2023/24 ($75,000 Wilkins Family Foundation + $25,000 Harvey Foundation)
Develop a living paediatric brain cancer biobank through processing of fresh tumour material (resected from children with brain tumours as part of their normal therapy) into patient-specific:
1. cell lines
2. organoids
3. patient-derived xenograft mouse models of paediatric disease.
Our focus will be on malignant paediatric brain tumours: medulloblastoma, high grade glioma (including anaplastic astrocytoma, diffuse midline glioma (DMG/DIPG) and glioblastoma) and ependymoma. The development and use of these models will facilitate better understanding of the drivers of tumour growth and resistance to current therapies, enable the discovery and evaluation of new therapies, and translation of this research into the clinic.

Funding: $150,000 over 3 years by the NRF Paediatric Fund commencing 2023/24
We wish to develop key facilities to expand paediatric brain cancer research in South Australia. To do this it is essential to establish a comprehensive, well annotated and run paediatric brain cancer biobank that will foster high quality discovery and clinical research. It is particularly important to have this paediatric brain cancer biobanking capacity established in South Australia as we move toward proton therapy for children with brain tumours at SAHMRI and the Bragg Centre for Proton Therapy and Research. We are seeking support to establish this important initiative.

Funding: $100,000 (James & Diana Ramsay Foundation)
We are developing a new treatment for glioblastoma, based on a revolutionary type of ‘living drug’ known as CAR-T cells. In this approach, T cells (part of our immune system) are isolated from a patient’s blood and genetically engineered to give them cancer killing activity. These cells are returned to the patient’s bloodstream; they then travel to the tumour to attack it from within. CAR-T cell therapies are targeted specifically toward cancer cells. This has the advantage of causing much less long-term toxicity and damage to healthy tissues as compared to chemotherapy or radiation.
To achieve our goal of developing successful CAR-T cell therapies for children with diffuse intrinsic pontine glioma, our team of scientists and doctors first test and optimise potential new therapies in the laboratory. LEVI’S-CATCH Clinical Trial of GD2-CAR-T is commencing at Sydney Children’s Hospital with 5 patients. A 6th patient is likely before year’s end.
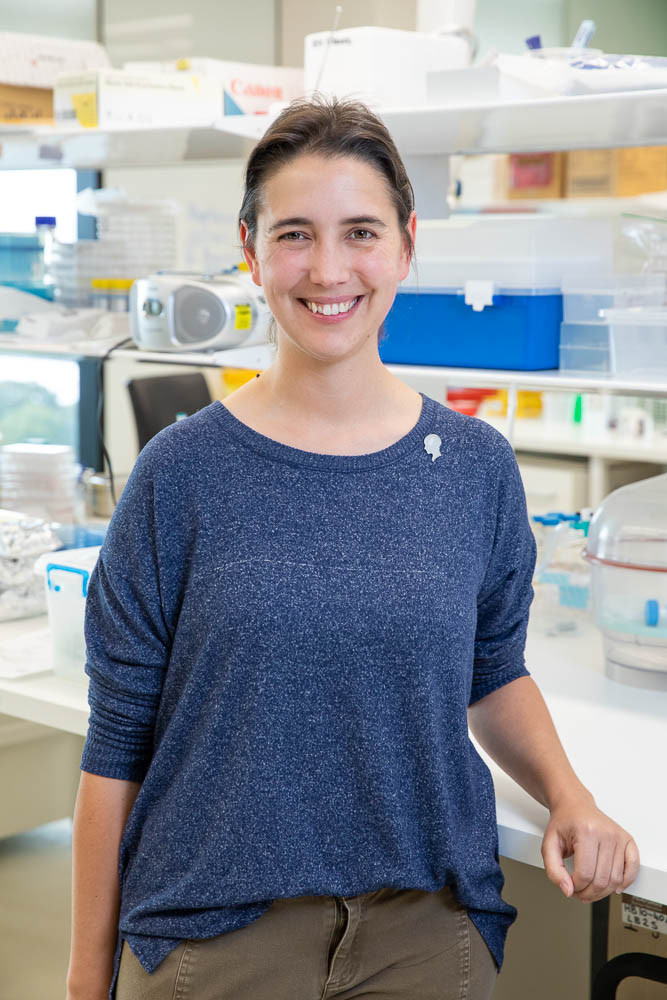
Dr Tessa Gargett, Research Officer
Centre for Cancer Biology, UniSA
Funding: $50,000 by the NRF Paediatric Fund
Diffuse intrinsic pontine glioma (DIPG) is the most common, aggressive and lethal of childhood brain cancers. The infiltrative and invasive nature of DIPG in the brain’s ‘junction box’ limits the effectiveness of potential treatments. Genetically engineering a patient’s own white blood cells against DIPG to make chimeric antigen receptor (CAR)-T cells is emerging as a promising new therapy. However, CAR-T cell therapy is not effective in all DIPG patients may induce adverse conditions. We have discovered a method that may overcome this limitation of CAR-T cell therapy.
Funding: $47,790
The proposed project aims to improve the treatment of paediatric brain cancer using advanced artificial intelligence (AI) technology. We are developing a system that will help doctors accurately identify and outline the critical areas of the brain during radiation therapy planning. By leveraging AI algorithms and analysing large datasets of brain images with tumours, we aim to automate and optimise this process, ensuring precise treatment targeting while minimising side effects. This innovative approach has the potential to enhance the effectiveness and safety of treatment, leading to better outcomes for children with brain cancer.

Funding: $35,000
Diffuse intrinsic pontine glioma (DIPG) is the most common, aggressive and lethal of childhood brain cancers. The infiltrative and invasive nature of DIPG in the brain’s ‘junction box’ limits the effectiveness of potential treatments. Genetically engineering a patient’s own white blood cells against DIPG to make chimeric antigen receptor (CAR)-T cells is emerging as a promising new therapy. However, CAR-T cell therapy is not effective in all DIPG patients. Soft outer cell membranes, which enable cancer cells to slither and invade in the brain, also prevent their killing by CAR-T cells, but can now potentially be stiffened by new drugs.
Funding: $29,388
Dr Gareth Rutter, Registrar
Women's & Children's Hospital
2021 Research Funded:
Funding: $50,000
Project: Diffuse intrinsic pontine glioma (DIPG) is the most aggressive childhood cancer and the leading cause of brain tumour-related death in children. Despite intensive research, effective treatments have not been developed other than use of radiotherapy to relieve brain tumour symptoms.
Here, we will extend our successful methods based on the genetic engineering of T cells to develop genetically engineered NKT cells. Unlike T cells, NKT cells are a white blood cell that can be modified to target both tumour cells and scavenger cells in the tumour microenvironment, thus potentially overcoming two factors responsible for aggressive tumour behaviour and therapy resistance.
Ms Kristyna Sedivakova
University of Adelaide - Translational Oncology Laboratory
2020 Research Funded:
Medulloblastoma is the most common malignant brain tumour in children, frequently occurring in early childhood before the age of five. Treatment for medulloblastoma involves surgical resection, radiation of the brain and spine, and chemotherapy. The five-year survival rates have improved over the last 20 years, however unsurprisingly, exposure of the developing brain to chemotherapy and radiotherapy has detrimental life-long side effects. These include neurological and auditory deficits, secondary cancers and hormonal dysfunction, as well as non-physical deficits such as learning difficulties and psycho-social issues. Therefore, new less toxic targeted therapies for medulloblastoma are desperately needed. We have identified a new therapeutic target for medulloblastoma, and new experimental drugs for this target that show great promise as a potential new therapy for medulloblastoma. Our aim is to assess this potential new therapeutic approach in advanced preclinical models of medulloblastoma. Successful outcomes will provide impetus for future clinical trials for medulloblastoma treatment.

Dr Mel Tea
University of South Australia, Centre for Cancer Biology
Funding: $50,000 – NRF Paediatric Research Fund – University of Adelaide
Project: Standard treatments for childhood brain cancers are unsatisfactory. The cancer cells grow back and cause death in almost all patients. Breakthrough treatments using engineered white blood cells have transformed survival prospects for patients with blood cancers. We want to extend the promise of this cell therapy to brain cancer patients. Here, we will combine our expertise in basic and clinical science to develop a new cell therapy program and so harness the power of the immune system to beat brain cancer.
Dr Tessa Gargett
Researcher, University of Adelaide/UniSA
Project: This project will investigate a potential therapeutic, an NK1 antagonist, which blocks the actions of the pro-inflammatory mediator substance P, which is present in higher levels in children. Substance P release causes ongoing neuronal injury and blocking its effects represents a novel mechanism for improving outcome.
Dr Frances Corrigan
Senior Lecturer, Division of Health Sciences, University of South Australia
Traumatic brain injury (TBI) is common during childhood and adolescence, with most injuries classified as mild (concussions), but these can still have long-lasting consequences. Indeed, the paediatric population take longer to recover from concussive insults than adults and report higher rates of impulsivity, attention deficits and cognitive impairment post-injury. This longer recovery may relate to ongoing brain development in this population. In particular the pre-frontal cortex which continues to mature into early adulthood is important for the development of executive functions which control judgement, planning, impulsivity, and working memory. As such the age of onset of a concussion may interrupt the normal maturation processes within this region leading to ongoing impairment of executive functions. This project aims to investigate whether the age at which a concussive impact occurs can have differential effects on the development of the pre-frontal cortex. This will be through examination of effects on executive function in adulthood- by examining impulsivity, working memory and judgement and linking this to changes in the key neurotransmitter systems within this region of the brain. Importantly this will be linked to magnetic resonance imaging (MRI) measures that will identify whether there are any signature alterations that can be linked to persistent behavioural changes.
Chief Investigator Team:

Assoc Prof Lyndsey Collins-Praino and Dr Frances Corrigan
University of Adelaide
Despite evidence to suggest that children and adolescents take longer to recover from a concussion and may be more vulnerable to long-term detrimental effects, the majority of concussion research has focused on adults. Little is understood about the scaling of these parameters required for paediatric pre-clinical models. The aim of this research program is to develop a new apparatus to impart a mechanically relevant concussive brain injury mechanism, which can be scaled for age, in a pre-clinical model.

Dr Claire Jones
Spinal Research Group & Centre for Orthopaedic and Trauma Research, Adelaide Medical School, NHMRC Early Career Research Fellow; Adjunct Lecturer, School of Mechanical Engineering, University of Adelaide
For children who survive childhood cancer, the burden continues, with up to 70% of survivors experiencing chemotherapy-induced cognitive impairment (CICI). CICI impairs attention, and memory, which profoundly impacts academic and social performance, as well as quality of life. To date, the brain changes that give rise to these impairments are unknown. In this study we will determine whether a specific type of inflammation in the brain contributes to CICI development over an acute and chronic time course. The results will facilitate development of targeted therapies for prevention of CICI, in addition to informing clinical assessment protocols and survivorship care plans.

Dr Alexandra Whittaker
Paediatric Brain Tumour Research, University of Adelaide
Our team is focussed on developing new therapies for brain cancer, based on a revolutionary new approach known as CAR-T cell therapy. This technique has already shown remarkable success in treating some forms of leukaemia. It involves collecting ‘killer’ T cells from a cancer patient’s own blood, and using genetic engineering techniques to make them specifically latch onto, and then kill, cancer cells. We are currently developing and testing CAR-T cells which specifically recognise brain cancer cells, and – with the support of organisations such as the NRF – hope to progress this work toward patient clinical trials within the next 5 years.
Dr Lisa Ebert BSc, PhD
The University of South Australia
Click here to donate to The Paediatric Appeal.